Our Services
Gastroenterology Dietetic Services
Andrew will ensure that your condition is fully evaluated to reach a rapid diagnosis so that carefully delivered, evidence based care, can be given, especially dietary advice and support.
Sian will provide you with this specialist evidence-based dietary advice, taking into consideration your lifestyle, energy expenditure and overall macro and micronutrient requirements.
Written resources will be provided to support you manage your digestive condition. Following your clinical dietetic assessment, you will be sent a copy of my letter sent to your referring Consultant. Your GP will also receive a copy of this.
The Gastroenterology Dietetic services we provide are:
Irritable Bowel Syndrome
Once you have had appropriate investigations undertaken by your Consultant Gastroenterologist, to confirm that IBS is the correct diagnosis you are likely to find considerable benefit from the Low FODMAP approach, which is helpful in 70-75% of IBS patients who will then be able to self-manage their symptoms in the long term.
Dr Millar, or your own specialist, will ensure that you receive the best treatment with other lifestyle changes and medical treatments when required.
Once you have identified your food intolerances, you will once again be able to enjoy cooking, family meals and eating out.
Some patients require a less formal approach then the FODMAPS diet, particularly when symptoms are mild or improving, and in this case we will offer the ‘first line’ dietary advice, based on National Institute of Clinical Excellence (NICE) guidelines.
You can read more information in the Irritable Bowel Syndrome and Diet fact sheet on the British Dietetic Association (BDA) website, on the ibsnetwork website and on The Guts UK website.
Begoodtoyourgut blogs on this subject include:
- Irritable Bowel Syndrome should I be taking probiotics and prebiotics?
- Lifestyle therapies to help in the management of Irritable Bowel Syndrome
- An introduction to the Low FODMAP diet
You may also want to consider looking at NHS Webinars on diet (https://patientwebinars.co.uk/condition/ibs/webinars/) and additional lifestyle information on the management of Irritable Bowel Syndrome.
Sian is fully trained as a Low FODMAP practitioner by the team at Kings College London. She also regularly attends update sessions undertaken by this team at Kings College and Guys and St Thomas’s Hospital, to ensure her knowledge and skills are regularly updated.
You will be provided with the latest resources produced by Kings College London, in association with Guys and St Thomas’s Hospitals, in addition to recipe suggestions and signposted to helpful apps to support you identify which foods are high in fermentable carbohydrates and which are suitable alternatives. Sian’s approach is holistic. She will provide guidance on activity/exercise and stress management strategies, in addition to diet, where appropriate.

Coeliac Disease
Coeliac disease affects all ethnic groups and is common in Europe and North America. It affects at least 1 in 100 people in the UK and in Europe; however, only about 24% of people with the condition are clinically diagnosed and this unfortunately can take on average a very lengthy 13 years.
The only treatment at present is lifelong adherence to a strict gluten-free diet. Obvious sources of gluten include flour and flour based foods, breads, pasta, cereals, cakes and biscuits. If a gluten-free diet is not followed, the disease can ultimately lead to nutritional deficiencies, osteoporosis, anaemia, cancer of the small bowel and unexplained infertility problems.
Following your diagnosis, a consultation with Sian will include an individual assessment of your current diet and equip you with practical advice on where to access gluten free foods, avoid food cross contamination, accessing gluten free restaurants/cafes, travelling overseas and avoiding where possible dietary deficiencies including iron, calcium and fibre.
Sian recommends patients consider joining Coeliac UK. It is a fantastic source of general advice, particularly additional dietary support: on all matters related to your disease, new food products as they become available, recipes and access to the excellent Food and Drink directory and GF Checker app which will help you when out shopping:
You can read more information on the Coeliac UK website or within the Coeliac Information entry on the Guts UK website.
Begoodtoyourgut blogs on this subject include:
NICE Quality Statement 5 (2016):
‘recommends considering the need for specialist nutritional advice as part of the patient’s annual coeliac review’

Inflammatory Bowel Disease
It is thought that there are around 240,000 people in the UK with inflammatory bowel disease These are lifelong conditions and most commonly first present in the teens and twenties. Men and women are equally affected.
Some patients with active disease can become undernourished as a result of an inadequate dietary intake, increased nutrient requirements and sometimes-excess losses due to poor digestive absorption, in association with drug interactions. People can also over restrict foods in an attempt to self manage their symptoms. Studies have shown that adult patients with Crohn’s disease can have lower levels of Vitamins D, K, Vitamins B1 and B6 and also zinc. Anaemia can also become an issue if there is intestinal bleeding and Vitamin B12 deficiencies can occur in some patients after surgery.
Some patients with Crohn’s disease have strictures identified, requiring them to limit fibrous i.e. pulses, fruits, vegetables and wholegrain foods. Lactose can also be poorly tolerated in some Crohn’s patients.
Sian will help provide you with clear guidance on optimising your dietary intake and provide you with effective, ‘evidence based ‘nutritional support strategies for managing your condition.
You can read more on Crohn’s and Colitis website on Crohn’s Disease on Ulcerative Colitis. Both of these can be accessed directly on the Guts UK website.
2013 Standards for the Healthcare of People who have Inflammatory Bowel Disease (IBD)
Standard A5 – ‘Access to a Dietician should be available to all IBD patients’.
2013 Standards for the Healthcare of People who have Inflammatory Bowel Disease (IBD)
Standard A5 – ‘Access to a Dietitian should be available to all IBD patients’.

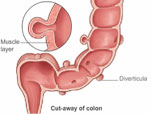
Diverticular Disease
This is the medical term used to describe the small pockets that stick out of the side of the large intestine (colon).
Diverticula are common and associated with ageing. One in four people who develop diverticula will experience symptoms, such as bloating and abdominal pain; other people will experience no symptoms at all. Diverticula are identified at colonoscopy or computerised tomography (CT scan).
Diverticulitis occurs when these pockets become inflamed or infected requiring prompt medical attention. If this is the case, it may necessitate a short period of time on a fluid and/or very low fibre diet.
People aged 50-70 who eat a high-fibre diet (25grams a day) have a 40% lower chance of admission to hospital with complications of diverticular disease – compared to others in this age range with the lowest amount of dietary fibre.
Most people with diverticular disease are however recommended to eat up to 30grams (1oz) of fibre a day.
Sian will advise you how to practically achieve a higher fibre diet (or in the case of severe diverticulitis, a fluid or very low fibre diet may be required in the short term), based on an assessment of your current intake of dietary fibre. You may find that you can tolerate certain fibres better than others for example soluble fibre – oats, fruits, vegetables and pulses. She will then aim to help you achieve an optimal amount of soluble and insoluble fibre daily, in addition to ensuring you have sufficient fluid in your diet.
Fibre supplements, usually in the form of sachets of powder that you mix with water may also be suggested.
You can read more information on the Fibre fact sheet on the British Dietetic Association (BDA) website or on the Diverticular Information section on the Guts UK website.

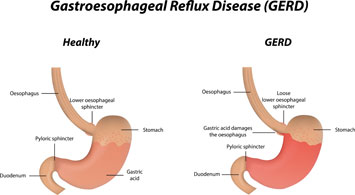
Gastro-oesophageal Reflux Disease (GORD)
It is very important that the underlying cause of your symptoms is fully investigated by your GP and Consultant. GORD is however a very common disorder affecting one in ten people on a weekly basis and can often improve with weight loss and other small dietary changes, including modification to eating behaviours, in association with antacids and low dose proton pump inhibitors.
Sian will ask you to fill in a food and exercise diary on our website, including your weight and height.
She would then arrange to speak to you either at BMI Cavell. If that is not convenient a Facetime or Skype consultation may be arranged.
You can read more in the Heartburn & Reflux information sheet on the Guts UK website or on the NHS Choices website.
Begoodtoyourgut blogs on this subject include:
Testimonials
What our clients have to say
I was initially referred to Mrs Shepherd following a diagnosis of IBS in 2012. At that time she introduced me to a low fermentable carbohydrate (FODMAP) diet which was a complete revelation. Within a three month period, I noticed a significant improvement in all of my symptoms and, with Mrs Shepherd’s professional expertise and guidance, […]DC
Teacher
Sian was my saviour through my treatment. She instilled so much confidence in me that I followed her advice on foods I could and could not eat. She is a professional and knowledgeable in her trade, her service was impeccable. I had regular consultations with Sian who also worked closely with Dr Karp, my oncologist. We were overwhelmed that my bloods were good, including my iron levels and blood cells. This was due to changes in my diet.SM
Higher Education Tutor
It was lovely to meet you today. I was so excited for your information that I instantly installed the ap. You have given me great hope and I feel it will work. You have such a wonderful way of doing your job and sympathising with what I am going through. Having met many doctors with my symptoms, I feel there is finally light at the end of the tunnel. I am just grateful Dr Miller recommended you.JS
Company Director
I visited Sian after being recommended by a gastroenterology consultant I have a non alcohol fatty liver. After my first session with Sian she introduced the idea that the cause may be that I binge eat. Having the open, honest and calming conversation with Sian really opened my eyes to my eating habits. She recommended a programme for me to improve my liver health and I now feel so much better. Thank you Sian for your coaching.CP
Local Government IT Consultant