Lifestyle therapies for management for IBS

Lifestyle therapies for management of IBS – exercise, cognitive behavioural therapy, relaxation techniques, mindfulness, yoga.
Irritable bowel syndrome (IBS) is a functional disorder of gut-brain interaction. It is no different to the majority of chronic conditions out there where lifestyle can play an important role in symptom management and improved quality of life. The cause of IBS is largely unknown. It is classified as recurrent abdominal pain, on average at least 1 day/week in the last 3 months, associated with two or more of the following:
- Related to defecation
- Associated with a change in frequency of stool
- Associated with a change in form (appearance) of stool.
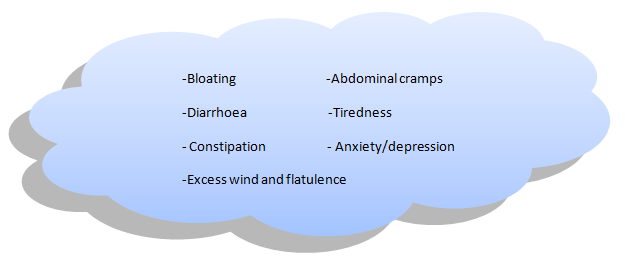
At any one time, IBS affects around 10-20% of people living in the UK. . A few common symptoms are outlined below:
There is no cure for IBS but you can learn to manage your symptoms.
Mind and Mood
 Many of those suffering with IBS will recognise the link to their mood and stress. Other common triggers include food, caffeine and alcohol triggering your symptoms but your mind and mental state should also be considered as a potential trigger.
Many of those suffering with IBS will recognise the link to their mood and stress. Other common triggers include food, caffeine and alcohol triggering your symptoms but your mind and mental state should also be considered as a potential trigger.
Research has shown that the severity of symptom onset in IBS is associated with something called gastrointestinal (GI)-specific anxiety -or GSA to make our lives easier. This describes those feelings of worry when not knowing where the nearest bathroom facility is or that feeling of fear when you experience GI sensations. Thankfully there has been increasing evidence demonstrating that lifestyle management can help.
Lifestyle management when I have IBS…What does this mean?
When managing IBS, it’s important to understand what’s going on and why. IBS is a complex motility and sensory disorder whereby a single piece of advice cannot be given to all. Different things will work for different people as the symptoms of IBS vary across individuals. This is why seeking help from a professional is vital; qualified to offer a treatment plan which is tailored to you and your lifestyle.
The word ‘’lifestyle’’ is used when referring to things in your life which you have control over. The beauty in lifestyle management is that you have control over the changes you make. For example, if your symptoms arise from increased stress, you can begin to address this through doing things which will help alleviate your stress levels (such as exercise, mindfulness meditation or yoga).
Mindfulness
There are various definitions of mindfulness out there. It’s commonly defined as a process of paying attention to the present moment in a non-judgemental manner. It can be considered a type of therapy which is all about our awareness. Mindfulness is thought to reduce anxiety-related symptoms in IBS – which is very common. There are different ways to practice mindfulness, such as a mindfulness-based stress reduction (MBSR) programme or mindfulness-based cognitive therapy (MBCT).
There has been encouraging evidence on the success of practicing mindfulness in IBS. A randomised controlled trial (Kearney, D. J, 2012). evaluated the effects of MBSR in 75 women, whom in which were split into two groups; intervention (MBSR programme) and control group. Measures such as IBS symptoms, IBS quality of life and GI-specific anxiety were taken immediately post-intervention and at a 3-month follow-up. Results showed that the women who were randomised to the MBSR programme had less IBS symptoms immediately after the intervention (26.4% vs 6.2%), as well as at a 3-month follow-up (38.2% vs 11.8%). Despite the study having a small, specific sample size, this study provides a good indication on the positive effect mindfulness can have in IBS patients.
 To find out more about mindfulness, check out these resources:
To find out more about mindfulness, check out these resources:
Mindful.org – https://www.mindful.org/meditation/mindfulness-getting-started/
NHS – https://www.nhs.uk/conditions/stress-anxiety-depression/mindfulness/
Headspace – https://www.headspace.com/
Calm – https://www.calm.com/
What about Yoga?
Yoga is seen as a state of balance between the body, mind and spirit. It originates back more than 5000 years ago in India and so as its benefits have been recognised for many years to say the least. Its original purpose was to heal a person through spiritual means. However, the basis of yoga is becoming more recognised today as its benefits range from reducing stress to improving depression and anxiety. Its aim is to slow down thoughts in order to understand what is going on. It can tap into areas which talking alone cannot. It can be thought as a key to open the depths of your thoughts.
Yoga exercises are designed to improve muscle tone, flexibility, and circulation as well as improving the well-being of the mind.
Yoga has been shown to reduce physical tension and may help to speed up recovery from stressful situations, relieve insomnia, improve concentration and energy levels. Local leisure centres and private studios providing classes are now available in many parts of the UK.
Many people with IBS use Yoga and meditation to find that peace of mind to quell the inner turbulence and manage their lives better which can have a positive impact on IBS symptoms.
E-E-Exercise!
Another way you can manage your symptoms is exercise. It seems as though exercise is the solution to nearly everything, and that’s because it (kind of) is. In IBS, exercising can help keep the digestive system moving. It can also be soothing for your mental state as endorphins are released (a chemical which helps reduce stress). A study (Johannesson et al., 2011) looked into the effects exercise has on IBS patients. It was found that patients who increased their exercise experienced a reduction in their symptoms in comparison to the control group whose symptoms worsened.
- Adults (19 – 64) should aim to exercise for a minimum of 150 minutes per week. of moderate aerobic activity such as cycling or brisk walking every week and also include some
- Strength exerciseson 2 or more days a week that work all the major muscles (legs, hips, back, abdomen, chest, shoulders and arms).
Depending on where you are, you can jazz up your exercise sessions by listening to your favourite music/podcasts, watch a TV programme or video in the gym or asking someone to join you for that park walk or run.
 Cognitive Behavioural Therapy (CBT)
Cognitive Behavioural Therapy (CBT)
CBT has recently been considered a treatment option for IBS. It is a type of psychotherapy which was first developed to treat mental health conditions such as depression and anxiety.
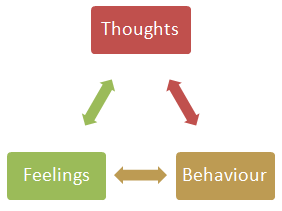
The idea behind CBT originates from the concept that our thoughts, feelings and behaviours are interlinked. In other words, having destructive thoughts will negatively impact how we feel and thus negatively impact how we behave. Through drifting our focus on where this negative chain starts from, CBT can improve our emotional state and our behaviour.
CBT and IBS…Medicine for the Mind
CBT might sound like as unusual way to ameliorate the severity of your symptoms, especially in a world where medication is the go-to! But, as important as medications and dietary changes are, equally so is therapy for the mind.
If you think about it, the mind is constantly working –even right now as you’re thinking about how it’s working, it is working! So it’s no surprise why CBT can sometimes be needed.
As mentioned earlier, the brain interacts with the gut which can result in unpleasant tummy grumbles. CBT can help in combatting the thoughts which lead to these tummy troubles through training our mind by engaging in activities such as breathing, muscle relaxation and guided imagery.
If you feel like you’ve tried everything, why not explore this option? CBT requires input from a qualified therapist, and cannot be done by anyone.
To access an accredited therapist, from either the British Association for Behavioural & Cognitive Psychotherapies (BABCP), which is the lead organisation for CBT in the UK and Ireland, or the Association for Rational Emotive Behaviour Therapy (AREBT), have a look at
For more information on this you can always drop our specialists Sian or Andrew an email. Please see the Contact page for details.
This blog written by Student Dietitian Sena Ali and edited by Sian Shepherd (Specialist Gastroenterology Dietitian) and Dr Andrew Miller (Consultant Gastroenterologist).
References:
Kearney, D. J. (2012). Mindfulness meditation for women with irritable bowel syndrome – evidence of benefit from a randomised controlled trial. Evidence Based Nursing, 15(3), 80–81. doi:10.1136/ebnurs-2012-100488
Johannesson, E., Simrén, M., Strid, H., Bajor, A. and Sadik, R. (2011). Physical Activity Improves Symptoms in Irritable Bowel Syndrome: A Randomized Controlled Trial. American Journal of Gastroenterology, 106(5), pp.915-922.
Tags: CBT, Cognitive Behavioural Therapy, Exercise and digestive health, Lifestyle management & IBS, Lifestyle Therapies for IBS Digestive Health, Mindfulness, Stress and digestion, Yoga
0 Comment
Leave a Reply