Bile salt malabsorption and irritable bowel syndrome (IBS) – symptoms, diagnosis, medical and dietary management

Sena Ali (Student Dietitian)
Edited by Sian Shepherd (Gastroenterology Dietitian) and Dr Andrew Millar (Consultant Gastroenterologist)
What is Bile?
Bile is a green-like fluid in our body containing bile acids, which are the result of the breakdown of haemoglobin, the vital ingredient of red blood cells. It is made by our liver and stored in the gall bladder. When we ingest fats, also known as lipids, these need to be broken down (digested) in our body. However, as fats are insoluble, we need bile to help break fats down. Bile has a key role in the emulsification of fats which enables them to be then absorbed by the intestine.
A simplified process of fat digestion is as follows:
- We consume a meal containing fat
- Our gallbladder contracts, squeezing bile into the small intestine
- Bile acids help emulsify the fat in the intestine allowing digestion
- Used bile acid passes in the last part of the small intestine (terminal ileum)
- Bile acids are reabsorbed in the ileum and transported back to the liver in the portal vein
- Bile acids are recycled up to 6-10 times each day
This process is known as Enterohepatic Circulation
 Bile Salt MAL-ABSORPTION
Bile Salt MAL-ABSORPTION
The word malabsorption originates from the Latin ‘’mal’’ meaning bad, ill, poorly, etc., and ‘’absorption’’ meaning ‘’a swallowing up’’.
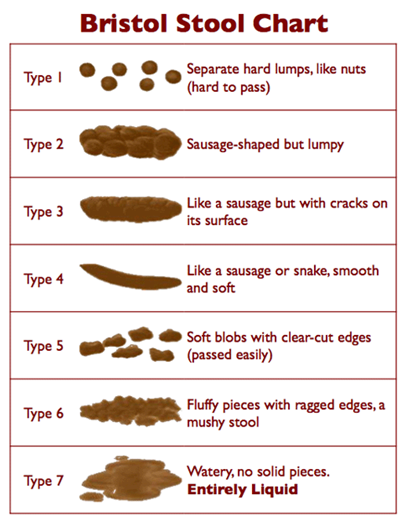
Bile salt malabsorption, also known as bile acid malabsorption (BAM) is a condition, which occurs when the intestines cannot absorb bile acid properly. Some call it Bile Salt Malabsorption (BSM). It happens because of a disturbance in the enterohepatic circulation. The result of this leads unabsorbed to ‘’leftover’’ bile entering the large intestine which then stimulates the secretion of water and electrolytes –resulting in diarrhoea and other symptoms such as bloating/cramps, abdominal pain, steatorrhoea and nocturnal defecation. Patients with this condition often report their stools to be type 6 or 7 from the Bristol Stool Chart (see here).
Causes
There is no single cause of Bile salt malabsorption. The different causes can be categorised as follows:
- Type 1: this is when there’s a problem in the terminal ileum. This can usually arise from inflammation, or related to a resection or removal of the ileum from perhaps a cancer treatment or Crohn’s disease treatment.
- Type 2: this is when there is no definitive cause found.
- Type 3: this is when there is another cause found, often associated with other gastrointestinal conditions like coeliac disease, chronic pancreatitis, cholecystectomy etc.
Bile Salt Malabsorption and IBS
Due to the nature of this condition, the symptoms present in bile salt malabsorption are often confused with IBS (in particular IBS-D). However BSM is often present in patients with IBS-D, perhaps because the rapid movement of the intestine moves bile into the colon before it can be reabsorbed. Unfortunately, in many patients with BSM the condition is not diagnosed leading to untreated symptoms poor quality of life. The cross-over comes from the fact that both conditions mirror similar symptoms, such as diarrhoea, bloating, lethargy, abdominal pain and excessive wind.
Diagnosis
The British Society of Gastroenterology and The National Institute for Health and Care Excellence have both published guidelines on the diagnosis of bile salt malabsorption. The diagnosis requires a test called a selenium-75 homocholic acid taurine (SeHCAT) test. It is a two-stage test. In the first part the patient swallows a capsule, which contains synthetic bile acids and a mildly radioactive powder. A scan carried out a week later identifies how much of the radioactive element has been retained and this indicates whether BSM is present. Some clinicians will use a medication, which absorbs bile acid to give an idea of whether the condition is present. This is called offering a therapeutic trial and can give an early indication of the diagnosis.
Treatment
The treatment of bile acid malabsorption can range from medical management with treatments to absorb bile acids to dietary modifications. It is also important to note that, if you have type 1 or type 3, managing any underlying conditions will improve overall symptoms.
Medical management
Medication which act as bile acid sequestrants are commonly prescribed for treatment. They are usually pills but can also come in powder form. They act by binding to the bile acid in the small intestine which prevents irritation to the large intestine and thus unwanted symptoms. See Table 1 below for the different types.
Table 1
| Bile Acid Sequestrant: | What is it? |
|
Cholestyramine and Colestipol |
These are commonly used as a first-line treatment. It is in a powder form, so it is therefore advised to mix in with a non-carbonated drink and to take by mouth. Due to the unpleasant taste, the tolerance and adherence to this medication is low. |
|
Colesevelam |
This is available in tablet form and therefore easier to administer. It appears to be well tolerated with flatulence and constipation being the most frequent adverse effects. In a RCT of 24 women with IBS-D, colesevelam did not provide any statistically difference compared with placebo (Odunsi-Shiyanbade et al. 2010). However Colesevelam did improve symptoms in people diagnosed with cancer and symptoms of bile acid malabsorption. It also resolved diarrhoea in 5 people with malabsorption whom in which cholestyramine was not tolerated well.
However, this medication is not licenced for this purpose in the UK. |
Dietary Modification
The use of a low-fat diet is an effective treatment to improve the symptoms present in this condition. This is because faecal bile acid excretion is increased with a higher intake of dietary fat. The intake of fat triggers bile secretion into the gastrointestinal tract. It is therefore advised to follow a low-fat diet to reduce symptoms caused by bile secretion. In essence, this means consuming 20% of total energy intake which equates to <40g of fat per day for women and <50g of fat per day for men. The guidance and support from a Registered Dietitian plays an integral role in the process of this treatment.
As fat also provide us with essential fat soluble vitamins (A,D, E and K), these can be substantially reduced on a low fat diet. Additionally, there maybe interference with the absorption of Vitamin B12 and so monitoring of these nutrients and supplementation may be required.
Reducing the intake of fat simultaneously reduces the total energy intake of the diet. It is important that this dietary energy balance is readdressed in association with a Registered Dietitian or Registered Nutritionist, particularly if you have high energy requirements secondary to your occupation (police, waiters, nurses/doctors, gardeners etc) or higher levels of physical activity due to sporting activity.
The majority of studies have assessed the effectiveness of a low-fat diet. A study on patients who had a 7-day SeHCAT scan result of <20%, carried out at the Royal Marsden Hospital, showed significant improvement. The study concluded that dietary intervention is an effective treatment option and should be routinely considered (Jackson et al., 2017).
It is important that an accurate diagnosis is made before treatment. Fortunately at BeGoodToYourGut, we can help you with both diagnosis and treatment with input from Sian, Specialist Gastroenterology Dietitian and Dr Millar, Consultant Gastroenterologist. If this is something you would like to consider, then you can do so by contacting them by clicking here.
This blog was written by Student Dietitian Sena Ali with review and further guidance from Sian Shepherd (Specialist Gastroenterology Dietitian) and Dr Andrew Millar (Consultant Gastroenterologist).
References:
- Odunsi–Shiyanbade, S., Camilleri, M., McKinzie, S., Burton, D., Carlson, P., Busciglio, I., Lamsam, J., Singh, R. and Zinsmeister, A. (2010). Effects of Chenodeoxycholate and a Bile Acid Sequestrant, Colesevelam, on Intestinal Transit and Bowel Function. Clinical Gastroenterology and Hepatology, 8(2), pp.159-165.e5
- Jackson, A., Lalji, A., Kabir, M., Muls, A., Gee, C., Vyoral, S., Shaw, C. and Andreyev, H. (2017). The efficacy of a low-fat diet to manage the symptoms of bile acid malabsorption – outcomes in patients previously treated for cancer. Clinical Medicine, 17(5), pp.412-418.
Tags: Bile salt malabsorption (BAM), Digestive disorders, Fat soluble vitamins, Irritable Bowel Syndrome, Low fat diet, SeHCAT test
0 Comment
Leave a Reply