Management Of Diverticular Disease

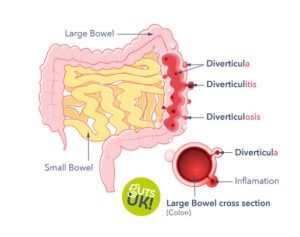
Diverticular disease and diverticulosis are digestive conditions that affects our large intestine. It is characterised by diverticula; which are small bulges that develop in the lining of our large intestine – our bowel – imagine the inner tube of a bicycle tyre bulging through the tread in the tyre.
The cause of diverticular disease is unknown, but risk factors include older age, low fibre diet, smoking, being overweight or obese, physical inactivity, history of constipation and/or long-term use of painkillers like ibuprofen.

Diverticular disease is usually asymptomatic. Around half of all older adults have some diverticulae and most of these will experience no symptoms. Some patients who have typical symptoms for IBS are found to have diverticular disease on imaging or endoscopy and naturally link the two conditions but these may be unrelated in many people.
About 10-15% of people with diverticulosis develop symptoms. Symptoms include tummy pain, constipation, diarrhoea and occasionally blood in poo. When symptoms are present, it is called diverticular disease. This is most commonly found on the left side of the large bowel (colon) but in people of Asian origin the diverticulae, and accompanying symptoms, may be right-sided.
A study in May 2020 indicated that probiotic treatment in this case Symprove, improved four symptoms albeit not abdominal pain, in adult patients, with moderate-to-severe disease. These patients were not however acutely unwell people with diverticular disease.
If the diverticula become inflamed or infected, which results in more severe symptoms such as constant severe tummy pain, high temperature, diarrhoea, or constipation and/ or blood in poo, it is called acute diverticulitis. The ending of the word diverticulitis means there is inflammation as in arthritis, sinusitis etc. If the inflammation is very severe it may cause an abscess to develop or even perforate. If severe infection happens urgent hospital treatment and possibly emergency surgery, is needed.
Reducing the risk and dietary management of diverticular disease
It is advised to consume a balanced, sustaining diet, which includes wholegrains, oats, fruits, and vegetables and pulses (peas and beans), there is no need to avoid seeds, nuts, popcorn or fruit skins. As mentioned before, a low fibre diet appears to be linked with developing diverticular disease and diverticulitis. Research has shown that fibre supports our large bowel functioning. These effects include increasing our stool output, diluting the colonic contents, and increasing the rate of the contents passage through our gut, making our stool softer and larger so they put less pressure on the walls of your intestines.

Eating a high-fibre diet may help ease the symptoms of diverticular disease and stop you developing diverticulitis. The recommendation is in line with national recommendations to aim to consume 30grams of fibre per day. This is important as currently in UK the daily average intake in females is 17.2g and males is 20.1g.
If your current fibre intake is low, it is recommended to increase fibre intake slowly incrementally, to avoid GI symptoms such as bloating, for example increase by 5grams per day to reach at least the government recommendation. This gives your gut time to adapt. Drinking adequate fluids also helps with the management of diverticular disease and side effects of high fibre diets.
Eating plenty of fibre supports our digestion and prevents constipation in addition to supporting other health benefits. For example, it is associated with reducing the risk of cardiovascular disease, Type 2 diabetes, and bowel cancer. Plus, a diet rich in fibre makes us feel fuller.
How can we increase our fibre intake?
- Consuming 5-a-day – frozen, tinned, fresh and dried fruit and vegetables all count!
- Including a portion of nuts or seeds into our diets – they make a perfect snack!
- Look at the labelling on food products, any product with the nutrition claim “high in fibre” contains at least 6g of fibre per 100g, and “source of fibre” contains at least 3g of fibre per 100g.
- Swapping white refined grains, to wholegrains.
- Choosing starchy foods such as porridge, oat bran, and potatoes with the skin on.

Dietary management of diverticular disease during an acute flare up/ infection (diverticulitis)
If you are diagnosed with diverticulitis, a GP may recommend a fluid-only diet for a few days and a very low-fibre diet to give your digestive system time to rest. This is the opposite of reducing the risk and management of diverticular disease. Further, if experiencing constipation, flatulence and bloating, a low-fibre diet may also be recommended temporarily to reduce these symptoms.
Once recovered and the symptoms have gone, it is then advised to gradually reintroduce a high fibre diet to personal tolerance, aiming again for 30g/ day in association with an adequate fluid intake.

Diagnosis / tests and monitoring of diverticular disease
Patients who describe symptoms which may be due to diverticular disease need careful assessment to ensure that other conditions are excluded, including bowel cancer, inflammatory bowel disease, irritable bowel syndrome and coeliac disease. A careful history and examination will be taken by a general practitioner, Gastroenterologist, Colorectal surgeon as needed. Invasive investigations are often not required but it is usually appropriate to carry out blood tests and stool tests. A stool test for microscopic blood, the qFIT test, will help to exclude malignancy and another, a faecal calprotectin, helps to exclude significant inflammation.
Some patients may require a scan, particularly if they have a severe flare up. A colonoscopy or CT colonography may be needed to exclude bowel cancer and to assess the severity of the diverticular disease.
Attacks of diverticulitis are usually accompanied by pain, a change in the pattern of the stool and sometimes with blood of signs of more severe infection, including a fever (high temperature), sweating and shivering. If you have signs of the latter these could be due to sepsis and immediate medical attention should be sought.
Treatment for attacks of diverticulitis will depend on the severity of the attack. Often resting, taking paracetamol-based pain killers (avoid Nurofen and aspirin) and keeping to a light/low fibre or fluid only diet, is sufficient to treat mild attacks. More severe attacks may require either oral or intravenous antibiotics and in serious cases an operation may be required.
Important Messages
- Diverticular disease is very common as we go older and often causes no problems at all
- Any new symptoms of pain or change in bowel habit should be discussed with your GP or a specialist. Appointments can be arranged with Dr Andrew Millar or Mr Lee Dvorkin to discuss your symptoms further.
- If you are seeking dietary advice to help you manage diverticular disease/diverticulitis, please contact Mrs Sian Shepherd.
- Urgent attention should be sought for symptoms with bleeding, progressive symptoms, or weight loss.
- Emergency treatment should be sought if there is severe pain or sepsis.
- Dietary management is very important with a high fibre diet being the most important and conversely an attack of diverticulitis, may necessitate resting the bowel with a soft/low fibre or liquid only diet.
Resources
- British Dietetics Association. Food Fact Sheets. Specially their one on “Fibre” and “Wholegrains” give great options of high in fibre foods, and wholegrain options.
- Fibre Fit App. This app allows you to put in what you are eating and will help you calculate how much fibre you are currently consuming.
- Guts UK information on diverticular disease. Guts UK is a national charity aimed at informing and supporting people with digestive diseases and funding research aimed at earlier diagnosis, kinder treatments, and ultimately, a cure.
- NHS website: Diverticular Disease.
References
https://www.nhs.uk/conditions/diverticular-disease-and-diverticulitis/
https://www.nhs.uk/live-well/eat-well/how-to-get-more-fibre-into-your-diet/
https://www.nature.com/articles/284283a0
https://www.bda.uk.com/resource/fibre.html
https://www.bda.uk.com/resource/fibre.html
https://www.bda.uk.com/resource/wholegrains.html
https://labellingtraining.food.gov.uk/module3/overview_3.html
https://cks.nice.org.uk/topics/diverticular-disease/
https://www.guidelines.co.uk/diverticular-disease-diagnosis-and-management/455109.article
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3625022/
https://www.nature.com/articles/nrgastro.2015.115#ref-CR5
The above blog has been written by ‘begoodtoyourgut.co.uk’ Emilia Fish, BSc A Nutr in association with Dr Andrew Millar, Consultant Gastroenterologist & Hepatologist and Mrs Sian Shepherd BSc RD – Specialist Gastroenterology Dietitian.
Tags: diverticula, Diverticular disease, diverticulitis, diverticulosis, Gut Health, high fibre diet, Prebiotics, probiotics, wholegrains
0 Comment
Leave a Reply